Do you avoid whole grains in fear of “wheat belly”? Have you been convinced whole grains are inflammatory foods?
Going against the grain seems to be gaining in exponential popularity these days. While I am not at all discounting everything the no-grain group is eating or endorsing, I do feel as though the time has come to discuss the ongoing bashing of whole grains.
Unrefined whole grains are NOT inflammatory foods. In fact, if you start doing a bit of research on PubMed, you’ll see the consumption of whole grains has not only been linked to decreased inflammation, but also to weight loss and gastrointestinal health, both of which many Paleo followers believe is not possible on a diet that contains grains.
But before we get to the grains, let’s chat a bit about the foods that are contributing to the rampant spread of a national inflammation epidemic.
The S.A.D. (Standard American Diet) is Rich in Inflammatory Foods
Almost half of all Americans suffer from an inflammatory disorder (and if you know my story, you know this includes me.) In fact, the common thread linking a tremendous number of seemingly unrelated conditions ranging from obesity to heart disease, asthma to allergies, fibromyalgia to arthritis, multiple sclerosis to endometriosis, and hundreds of others, is inflammation. The bad news is, so many of the foods that make up the S.A.D. (Standard American Diet), such as baked goods made with refined flour (crackers, pretzels, breads, pizza dough, etc.), sugar, meat, cheese, fried foods, and refined vegetable oils (corn oil, soybean oil, “pure” vegetable oil, etc) are all inflammatory foods that exacerbate whole-body inflammation and contribute to the worsening of a countless number of inflammatory conditions that affect millions of Americans.
The good news is, so many of the inflammatory conditions people suffer with can be dramatically improved simply be adopting an anti-inflammatory diet.
And really, whether you have an inflammatory condition or not, eating fewer inflammatory foods and more anti-inflammatory foods is something everyone can benefit from, including kids. Since all anti-inflammatory foods happen to be nutrient-dense, I actually can’t think of single person who would not benefit from eating an anti-inflammatory diet.
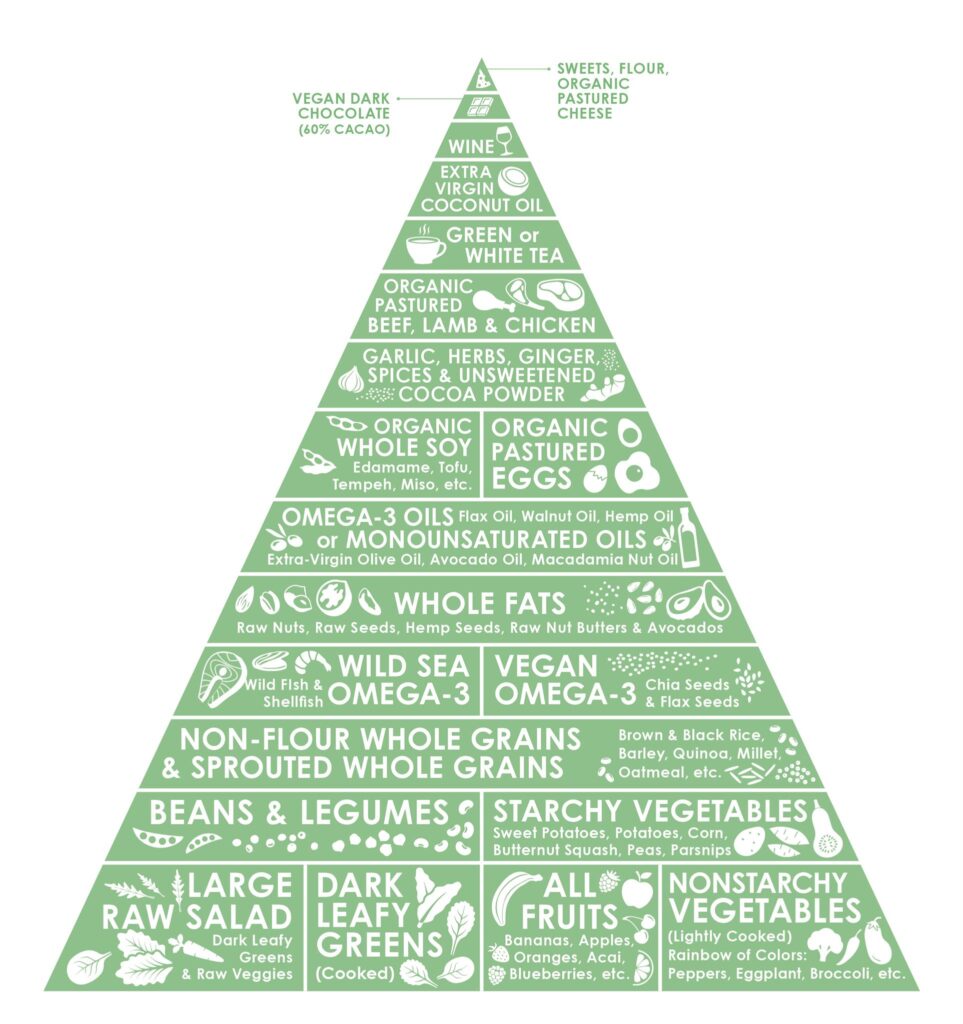 After looking at our Clean Cuisine food pyramid you will notice whole grains are not on the bottom of the pyramid (meaning we don’t suggest whole grains make up the bulk of your diet), but they certainly are not at the top of the pyramid either.
After looking at our Clean Cuisine food pyramid you will notice whole grains are not on the bottom of the pyramid (meaning we don’t suggest whole grains make up the bulk of your diet), but they certainly are not at the top of the pyramid either.
So, why then are whole grains wrongfully being labeled as inflammatory foods and getting such a bum rap these days?
Before we get down to the nitty gritty of whole grain nutrition research as it relates to inflammation, it is important to understand that the type of inflammation we are referring to is chronic, “whole body” systemic inflammation that manifests itself in the cardiovascular system and autoimmune system. This type of inflammation can be tested using standard biomarkers of inflammation with simple blood tests that measure such things as CRP (C-reactive protein), interleukin-1 and TNF (tumor necrosis factor).
Many studies show that lifestyle modification, including changes in diet, exercise and even nutrition supplementation with multi-vitamins (1) and fish oil (2) can reduce “whole body” inflammation. A diet high in fiber, with a favorable omega-3 to omega-6 ratio, reduces inflammation (3) as does eating plenty of phytonutrient-rich and antioxidant-rich plant based foods.
It also is well established in the medical literature that diets high in animal-based saturated fat and trans fats increase overall levels of inflammation (4), as can eating too many processed foods and too many calories in general.
In fact, even being overweight in and of itself will increase inflammation because fat cells are active and actually promote whole-body, chronic inflammation. To make matters worse, a viscous cycle exists where inflammation promotes more fat cells and the fat cells then promote additional inflammation. This terrible cycle is how some people wind up very overweight and highly inflamed. Also, keep in mind that any diet that helps you lose weight will indirectly help lower inflammation.
Where Do Whole Grains Fit In an Anti-Inflammatory Diet?
But back to whole grains. Where exactly do whole grains fit in? Before we look at individual studies showing how whole grains are not in fact inflammatory foods, it is important to point out that whole grains are an excellent source of key nutrients including iron, magnesium, B vitamins and vitamin E. Whole grains also contain an abundance of anti-inflammatory phytonutrients (by the way, phytonutrients are only found in plant-based foods) and antioxidants. Both phytonutrients and antioxidants help reduce oxidative stress, which indirectly reduce inflammation.
Whole grains are also key source of fiber, which plays an important role in reducing inflammation. In fact, simply increasing intake of fiber has been shown to lower inflammation and C-reactive protein (5). Keep in mind that the average American only consumes about 15 grams of fiber a day, which is roughly half of what is recommended. Since whole grains are one of the best sources of dietary fiber, banishing this food group from your diet makes meeting the optimal daily dietary fiber quota unnecessarily difficult.
And really, there is no reason you should be going out of your way to eliminate whole grains from your diet….
Whole Grains Reduce Inflammation, Promote Gut Health and Decrease Body Fat
If you have tried low-carb diet trends that drastically limit carbohydrate foods such as whole grains, it is highly unlikely that you are getting enough fiber, which not only plays an important factor in reducing inflammation, but also disrupts the probiotic conditions of your gut. In fact, researchers have found that eating whole grains (barley, brown rice, or especially a mix of the two) even for a short period of time favorably altered the gut microbiota in ways that coincided with improvements in systemic inflammation. (6) Whole grains rich in soluble fiber (such as oatmeal and barley) are also rich in prebiotic inulin and oligofructose, which feed the hungry probiotic bacteria in your gut. This special type of fiber helps temporarily trap carbohydrates in your digestive system and slow their absorption, which in turn curbs appetite and plays a critical role in promoting hunger-free weight loss. Another type of fiber found in whole grains, insoluble fiber (such which is found in whole wheat) promotes gut health by excreting bile in the small intestine, thus making the way for probiotic bacteria to enter the colon safe, sound and alive.
It is highly ironic that whole grains are often bashed for not being “gut friendly”, when in reality they play a tremendous role in promoting overall gastrointestinal health. It is well established that many dietary components can positively affect gastrointestinal health, including fiber, oligosaccharides, resistant starch, phytonutrients, antioxidant vitamins, and minerals and whole grains provide ALL of these beneficial components.
For the record, gastrointestinal health is characterized as maintenance of homoeostasis of gastrointestinal function by promoting efficient digestion, optimal gut immune responses, minimal inflammation, and the absence of disease. Currently, colorectal cancer is the 4th most common type of cancer, contributing to 53% of all gastrointestinal cancers (7), and happens to be a cancer for which my husband operates on routinely. Both epidemiological studies and prospective studies have shown an inverse association between whole grain consumption and the risk of colon cancer.
Although the starch in whole grains is often viewed as “bad” and pro-inflammatory, the reality is a portion of the starch in whole grains is not even digested your body resists the calories, hence the term “resistant starch.” Studies show a diet rich in resistant starch helps control blood sugar levels and reduce fat storage after meals as well as help you feel more full, so you eat less. (8) If you replaced the same number of meat and dairy calories with resistant-starch-rich whole grain calories, you would lose weight because not all of the whole grain calories would be digested or usable by your body. As discussed earlier, if you lose weight, you further decrease inflammation. Additionally, the resistant starch present in whole grains has been shown to play an important role in increasing beneficial bacteria and decreasing pathogens as well as decreasing the production of toxic metabolites (9). Along with the resistant starch, oligosaccharides present in whole grains selectively increase beneficial bacteria in the gut, mainly bifidobacteria and lactobacilli.
Beyond gut health, whole-grain consumption has also been linked with fewer deaths from an inflammation-related condition. Compared with women who rarely or never ate whole-grain foods, studies have shown those who had at least two or more servings a day were 30 percent less likely to have died from an inflammatory disease (10)
Whole grain consumption has also been linked to reduced levels of C-reactive protein (an important inflammation marker) in a number of studies. A randomized controlled crossover trial with 44 overweight or obese adolescent girls was done in order to gauge the impact of whole grain consumption on markers of systemic inflammation. After a two-week run-in period, half the girls ate a diet where at least half their grains were whole grains, while the others avoided whole grains entirely in favor of refined grains. After six weeks, both groups observed a four-week washout period, then the groups switched. When the girls ate whole grains, C-reactive protein reduced by an average of 21.8%; when they ate refined grains, CRP went up about 12.1%. Other inflammation markers were also significantly reduced during the whole grain period (11). Another study found women who ate even small amounts of whole grains—up to one serving a day–had, on average, 11.5% lower concentrations of CRP in their blood. Women eating a full serving (16 grams of a 100% whole grain food, in this study) or more of whole grain had, on average, 12.3% lower CRP levels (12). Epidemiological studies also provide support for an association between diets high in whole grains and lower C-reactive protein (CRP) concentrations. After adjusting for other dietary factors, each serving of whole grains is estimated to reduce CRP concentrations by approximately 7% (13).
In Conclusion
When it comes to determining whether an individuals diet is healthy or not, one must always look at the overall dietary pattern as a whole, rather than to focus on isolating individual components. For example, I consider myself an overall clean eater, but I do still eat a bit of cheese and I do still indulge in dessert—yet still, I manage to maintain healthy weight, I have favorable low blood pressure, my triglycerides are low, my CRP levels are low, my cholesterol is within a healthy range (and more importantly, my “good” HDL is favorably high.)
The point is, my overall diet is clearly working and is clearly managing to keep my inflammatory markers in check. However, I cannot attribute my good health to any one single thing I eat or do—it is the combination of everything that gets results. The same logic can be applied to whole grains. I cannot say with certainty whether it is the micronutrients such as folate and vitamin B-6, the polyphenols and antioxidant compounds, the phytonutrients, the probiotics or the fiber in whole grains that reduce oxidative stress and decrease inflammation. In all likelihood, it is the unique combination of all of these factors working synergistically that make the consumption of whole grains desirable as part of any healthy lifestyle, including one intended to decrease inflammation. In other words, it is the sum of the part of whole grains that promote good health.
References:
1. Church TS. “Reduction of C-reactive protein levels through use of a multi-vitamin.” Am J Med. 2003 Dec 15;115(9):702-707.
2. Maroon JC, Bost JW. “Omega-3 fatty acids (fish oil) as an anti-inflammatory: an alternative to nonsteroidal anti-inflammatory drugs for discogenic pain.” Surg Neurol. 2006 Apr;65(4):326-31.
3. Esposito K, Pontillo A, Di Palo C. Giugliano G, Masella M, Marfella R, Giugliano D. “Effect of weight loss and lifestyle changes on vascular inflammatory markers in obese women: A randomized trial.” JAMA. 2003 Apr 9;289(14):1799-1804.
4. Mozaffarian D, Pischon T, Hankinson SE, Rifai N, Joshipura K, Willet WC, Rimm EB. “Dietary intake of trans fatty acids and systemic inflammation in women.” Am J. Clin Nutr. 2004 Apr;79(4):606-612.
5. Ajani UA, Ford ES, Mokdad AH. “Dietary fiber and C-reactive protrein: findings from national health and nutrition examination survey data.” J Nutr. 2004 May;134(5):1181-1185.
6. Martinez I, Lattimer JM, Huback KL, Case JA, Yank J, Weber CG, Louk JA, Rose DJ, Kyureghian G, Peterson DA, Haub MD, Walter J. “Gut microbiome composition is linked to whole grain-induced immunological improvements.” ISME J. 2013 Feb;7(2):269-80. doi: 10.1038/ismej.2012.104. Epub 2012 Oct 4.
7. Altekruse SF, Kosary CL, Krapcho M, Neyman N, Aminou R, Waldron W, Ruhl J, Howlader N, Tatalovich Z, et al. , editors SEER Cancer Statistics Review, 1975–2007, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2007/, based on November 2009 SEER data submission, posted to the SEER Web site; 2010. [cited 2010 Jun 1]. http://seer.cancer.gov/statfacts/html/colorect.html#prevalence
8. C.L. Bodinham, G. S. Frost, and M.D. Robertson, “Acute Ingestion of Resistant Starch Reduces Food Intake in Healthy Adults,” British Journal of Nutrition 103, no.6 (2010):917-22.
9. Topping DL, Clifton PM. Short-chain fatty acids and human colonic function: roles of resistant starch and nonstarch polysaccharides. Physiol Rev 2001;81:1031–64 [PubMed]
10. Jacobs DR, Jr., Andersen LF, Blomhoff R. Whole-grain consumption is associated with a reduced risk of noncardiovascular, noncancer death attributed to inflammatory diseases in the Iowa Women’s Health Study. American Journal of Clinical Nutrition. 2007; 85:1606-14.
11. Hajishemi et al. “Whole grain intake favorably affects markers of systemic inflammation in obese children: A randomized, controlled, cross-over trial.” Molecular Nutrition and Food Research. 2014 Jan 20.
12. Journal of Nutrition. September 2010; 140(9):1669-1676. doi: 10.3945/jn.110.124164
13. Lefevre M, Jonnalagadda S. “Effect of whole grains on markers of subclinical inflammation.” Nutr Rev. 2012 Jul;70(7):387-96. doi: 10.1111/j.1753-4887.2012.00487.x. Epub 2012 May 22.








Dev Miller
Saturday 17th of January 2015
Hi Ivy, What's your take on the phytic acid that is naturally found in whole grains? As one of the "antinutrients" that blocks absorption of vitamins and minerals, I've read that it is important to break the acid down by processing whole grains properly prior to eating (soaking, sprouting or fermenting). Thanks and looking forward to your input!
Ivy Larson
Saturday 17th of January 2015
Hi Dev! Great question!! First of all, sprouting absolutely helps you absorb all of the vital nutrients stored within whole grains, so it really is the BEST option for eating whole grains.
But, having said that, I would not avoid whole grains just because they have not been sprouted.
Here's the deal: the phytates (and phytic acid) found in whole grains, legumes, nuts and seeds are actually antioxidant compounds. The chief concern about phytates is that they can bind to certain dietary minerals including iron, zinc, manganese and, to a lesser extent calcium, and slow their absorption. It might be true that if you ONLY ate whole grains and did not consume other whole foods that maybe the phytates might pose a problem (but you would run into problems if all you ate was say meat---one huge nutrition problem with eating a meat-only diet is that the animal protein would leach calcium from your bones)----the point is, you don't want to overdo any one single food group. But, the phytic acid found in whole grains eaten in their WHOLE form (which is not the same as say, supplementing your diet with wheat bran, which is just the fiber isolated from the whole grain) will not "steal" nutrients away from you. In fact!! Phytic acid has been shown to be healthful and beneficial. Phytates have been shown to have anti-inflammatory benefits and have been shown to help normalize cell growth and stopped the proliferation of cancer cells. They also may help prevent cardiovascular disease and lower a food's glycemic load. This is a great article that gives more detailed explanation---and if you scroll to the bottom you will see a link to click on all the references. http://www.precisionnutrition.com/all-about-phytates-phytic-acid
The bottom line though is that phytates in your everyday meals should not be an issue for you as long as you're eating a balanced diet. Most of us consume enough minerals in common foods to more than make up for the small amounts of these micronutrients that might be tied up by phytates. The only people who might need to be careful are vegetarians who consume a lot of wheat bran, which is a concentrated source of these substances. Phytate-associated deficiencies of iron and zinc do occur in some third-world countries where people mostly eat grains (but that is not at all what we recommend on Clean Cuisine--we suggest people eat about one or two servings a day of whole grains and we never suggest people take fiber supplements, wheat bran, etc.) Also, keep in mind that cooking reduces a food's phytic acid content to some degree, as does sprouting. Hope this helps?